Wisdom Teeth: The Final Frontier of Dental Development
Wisdom teeth typically emerge between the ages of 18-30, representing the final set of molars in the dental sequence. These third molars erupt into the oral cavity at varying positions and angles, often causing significant discomfort, inflammation, pericoronitis, and decay in adjacent teeth.
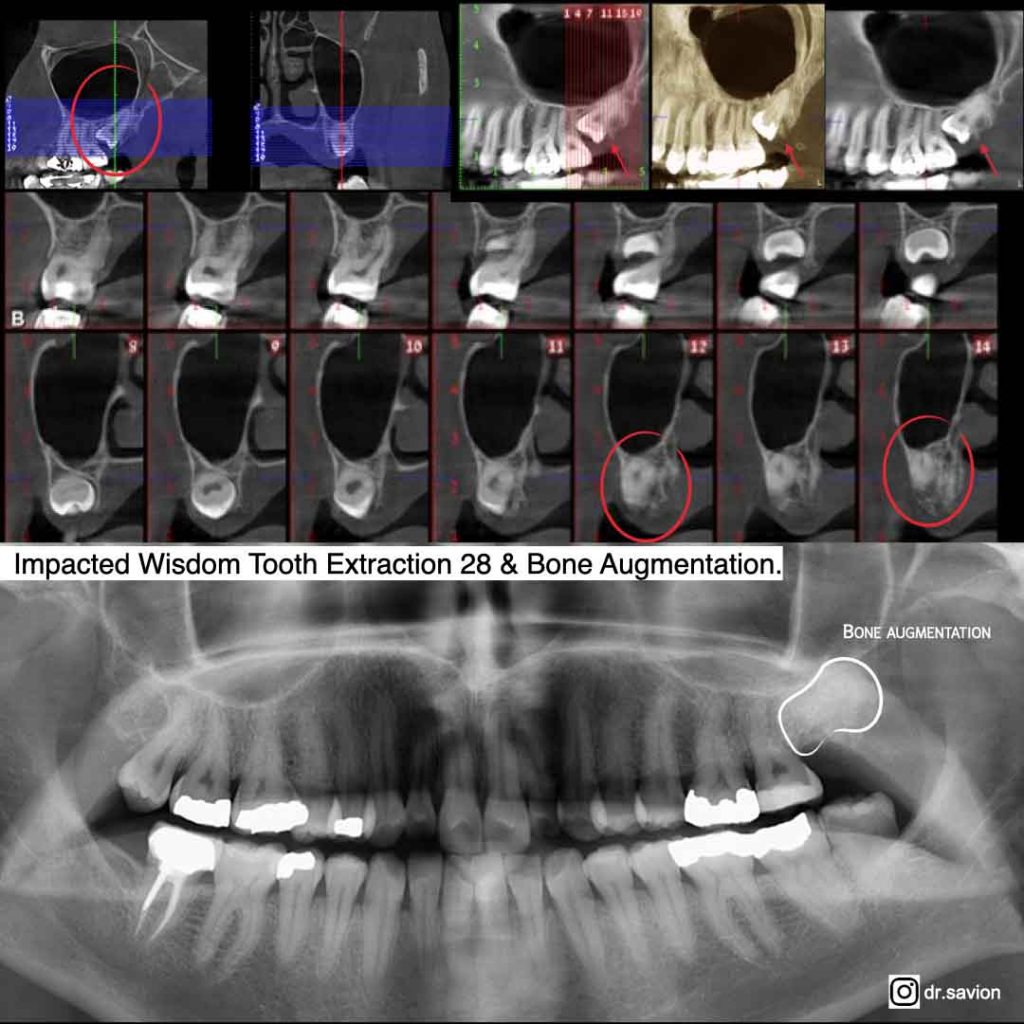
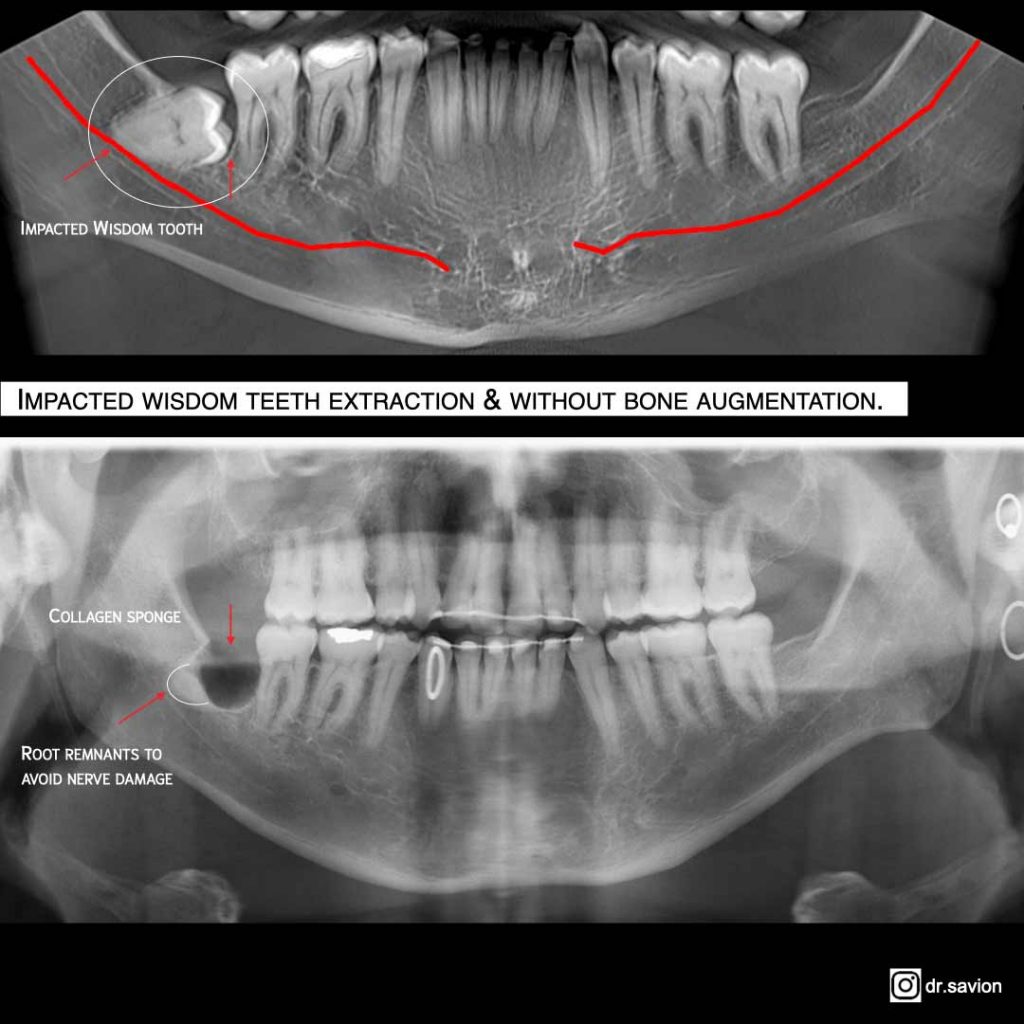
An impacted wisdom tooth refers to a tooth that fails to fully erupt or emerges only partially into the oral cavity, often in a mesial or distal position. This creates pressure on surrounding teeth and frequently results in severe pain, swelling, and periodontal pocket formation.
Dr. Ariel Savion has been an active dentist since 2007 and holds a dual Master’s degree from Germany in Laser Sciences and Dental Implantology. He has clinical expertise in laser periodontal therapy, microscopic surgery, and dental implant procedures.
He serves as the Medical Director of the dental corporation Savion Medical Center Ltd. and is the founder and owner of the prestigious master_implant educational club, dedicated to training dentists in advanced fields of dentistry.
In addition, Dr. Savion is the only certified instructor in Israel on behalf of the World Clinical Laser Institute in the field of laser dentistry.
Dr. Savion is an international researcher and lecturer and serves as a Key Opinion Leader (KOL) for leading medical companies in Israel and worldwide, specializing in laser dentistry, periodontology, and dental implantology.

Clinical Complications Associated with Wisdom Teeth
Wisdom teeth, also known as third molars, can cause a diverse range of complications when they emerge or fail to erupt properly.
- Impacted Wisdom Teeth: This represents the most prevalent complication. When wisdom teeth lack sufficient space in the jaw to erupt properly, they become trapped beneath the gum line or jawbone, leading to pain, swelling, and infection. Impacted wisdom teeth can also damage adjacent teeth, causing decay and infection. In certain cases, surgical extraction of the impacted wisdom tooth may be necessary to prevent further complications.
- Crowding: The eruption of wisdom teeth can cause crowding and occlusal problems when insufficient space exists in the jaw to accommodate them. This can result in the displacement of other teeth, causing discomfort and increasing the risk of periodontal disease and caries.
- Infection: Partially erupted wisdom teeth can create a "flap" of gingival tissue where food particles and bacteria accumulate, leading to inflammation and infection known as pericoronitis. This condition causes pain, swelling, and difficulty opening the mouth.
- Caries: The posterior location of wisdom teeth makes them difficult to reach and clean properly, making them more susceptible to decay and periodontal disease.
- Cysts and Tumors: Although rare, wisdom teeth can develop cysts or tumors in the surrounding tissue, potentially damaging adjacent teeth and bone structures.
Why and when is it recommended to have a wisdom tooth extracted?
Impacted wisdom teeth creating pressure on adjacent teeth and potentially causing cascading problems in the gums and jaw. Wisdom tooth extraction is typically recommended when symptoms appear such as:
- Pain
- Swelling
- Infection and inflammation
- Decay
- Orthodontic complications
- Bacterial accumulation sites that promote caries development. Extraction is often recommended due to their location—erupting last and positioned at the extremes of the jaw, making proper brushing and flossing challenging
- Additional complications that negatively impact the patient's quality of life.
Clinical Symptoms of Impacted Wisdom Teeth
An impacted wisdom tooth is one that cannot fully erupt, or erupt at all, through the gingival tissue. This condition can manifest through various symptoms:
- Pain: Pain represents one of the most common symptoms of impacted wisdom teeth. The discomfort can be dull or sharp and may be felt in the jaw, near the impacted tooth, or in surrounding teeth.
- Swelling: Impacted wisdom teeth can cause swelling of the surrounding gingival tissue, resulting in discomfort and localized inflammation.
- Jaw Stiffness: An impacted wisdom tooth can cause jaw stiffness and difficulty opening the mouth fully.
- Difficulty Chewing: Impacted wisdom teeth can cause pain and swelling that affects chewing ability.
- Halitosis: Partially erupted wisdom teeth can trap food particles and bacteria, leading to bad breath.
- Headaches: Impacted wisdom teeth can cause headaches and ear pain, particularly when the impacted tooth is located near the sinuses.
Causes of Wisdom Teeth Impacted
- Insufficient Space: The most common cause of impacted wisdom teeth is inadequate space in the jaw. When there isn't enough room for the tooth to emerge properly, it may become trapped beneath the gum tissue or jawbone.
- Abnormal Tooth Development: Wisdom teeth sometimes develop at an unusual angle or position, which can prevent them from erupting in a straight, normal manner.
- Obstruction: Since wisdom teeth are the last to emerge, they may become blocked by other teeth or bone structures, preventing them from having adequate space to erupt properly.
- Gum Disease: Periodontal disease can cause inflammation and swelling, which may make it difficult for wisdom teeth to erupt normally.
Diagnostic Imaging Requirements for Wisdom Teeth Assessment
The type of imaging required depends on the specific purpose of the examination. Generally, several types of imaging may be necessary for various dental procedures and treatments:
- Dental Radiographs: a. Intraoral radiographs taken inside the mouth provide detailed images of teeth and gums, allowing assessment of wisdom teeth positioning and surrounding conditions. b. Extraoral radiographs, taken outside the mouth, capture images of the face, jaws, and neck to evaluate jaw and facial structure.
Panoramic Radiographs: These provide a wide-angle view of the teeth, jaws, and surrounding structures, enabling comprehensive evaluation of wisdom teeth positioning and their impact on adjacent structures.
CT Scans: Three-dimensional imaging provides detailed pictures of teeth and jawbones, offering precise assessment of wisdom teeth location and their effect on surrounding teeth and structures.
Laser wisdom tooth extraction by Dr. Ariel Savyon:
Treatment Options for Wisdom Teeth
| Recommended Treatment | Clinical Situation |
|---|---|
| Regular monitoring and periodic check ups | Wisdom teeth do not cause pain or discomfort |
| Prolonged antibiotic therapy with adjunctive anti-inflammatory medication | Wisdom tooth is causing partial eruptions with inflammation and swelling of surrounding gum tissue |
| Antibiotic therapy to reduce inflammation | Gum infection around the tooth |
| Extraction | Tooth is impacted or causing pain |
Treatment approaches for wisdom teeth depend on the specific condition and severity of the problem.
- Monitoring: If wisdom teeth aren't causing any problems, your dentist may recommend regular monitoring to ensure they don't damage adjacent teeth or gums. This may require periodic dental examinations and X-rays to track the teeth.
- Crown Lengthening: If a wisdom tooth has partially erupted but remains covered by gum tissue, crown lengthening may be recommended. This procedure involves removing a portion of the gum tissue to expose more of the tooth, allowing for better cleaning and maintenance.
- Orthodontic Treatment: In certain cases, orthodontic therapy may be necessary to address problems caused by wisdom tooth eruption and to allow them to emerge properly.
- Antibiotic Therapy: If wisdom teeth are causing infection or inflammation, your dentist will prescribe antibiotics to reduce inflammation and prevent infection spread.
- Extraction: When wisdom teeth are impacted, extraction is often necessary. Even if they're not impacted but frequently cause pain, swelling, or other symptoms, removal may be required.
The Revolutionary Combination of Microscopic Approach and Laser Dentistry - Transforming Tooth Extraction
The integration of innovations and advanced technologies in various dental treatments, including tooth extraction, offers patients safer, faster, and more comfortable treatment options. One such groundbreaking innovation is microsurgery through the combination of therapeutic microscope use with various types of lasers.
This innovative approach has redefined the way dental treatments are performed. The combination of a dental microscope – offering enhanced magnification and precision – together with various types of lasers, such as diode lasers or erbium lasers, enables dentists to perform complex dental procedures with a level of accuracy that was previously unattainable.
The use of lasers in dental microsurgery allows for minimally invasive procedures, as the focused light energy can precisely remove tissue with minimal damage to surrounding areas. Lasers also have a cauterizing effect, helping to reduce bleeding, promote faster healing, and minimize post-procedural discomfort for patients. This innovative combination has revolutionized dental care, enabling a new level of efficiency in oral healthcare.
The combination of microscopic approach with laser dentistry is a winning formula because it harnesses the diagnostic precision of microscopy with the treatment accuracy of laser technology, significantly improving the dental process of tooth extraction and removal, including complex cases of impacted wisdom tooth extraction.
The microscopic approach in dentistry involves the use of high-powered dental microscopes, allowing the dentist to magnify the surgical area view, thereby enabling precise visualization of the tooth and surrounding tissues. These microscopes offer magnification ranges from 3x to 39x the natural tooth size, enabling dentists to identify even the smallest anatomical structures, as well as hidden fractures or infections that were previously undetectable.
This advanced form of dentistry requires considerable skill from the dentist, as the ability to see details in the treatment area with greater precision has led to the replacement of traditional dental instruments and drills with even smaller, more precise tools, enabling highly accurate dental treatments and offering additional benefits:
With the enhanced visibility provided by the microscope, a dentist can accurately assess the scope of the problem and avoid over-treatment. This is not only beneficial for the patient's oral health but also provides cost savings.
The microscopic approach enables treatment at a high level of precision, helping to preserve healthy tooth structure and surrounding tissues while reducing the risk of potential complications.
The use of a dental microscope allows skilled dentists complete control over the procedure. Enhanced visibility ensures no surprises during treatment, leading to predictable and successful outcomes.
Microscope-assisted dentistry allows the doctor to perform small, non-invasive surgical procedures with minimal trauma to soft tissues. This minimizes discomfort and pain during and after the procedure and shortens recovery times.
The use of laser technology has also revolutionized dental treatments; it offers an efficient, precise, and less invasive approach to various dental procedures. The use of dental lasers, which emit focused light energy, provides a wide range of applications that have changed and improved the way dental treatments are performed.
One of the most significant impacts of laser technology in dentistry is its ability to improve the efficiency and comfort of common procedures. While traditional treatment of impacted wisdom tooth extraction previously involved a surgical procedure requiring incisions, sometimes bone removal, and sutures (usually accompanied by a recovery period with side effects including pain, swelling, bleeding, and more), the introduction of laser technology has provided dentists with a minimally invasive alternative for impacted wisdom tooth extraction. The use of dental lasers helps in the precise and gentle removal of gum tissue and bone blocking the wisdom tooth. The laser beam simultaneously seals blood vessels and nerve endings, reducing bleeding and post-surgical pain.
The synergy of these advanced technologies, integrated in the dental clinic and operated by skilled hands, makes successful and painless dental treatment a reality.
10 Advantages of Wisdom Tooth Extraction Using Advanced Microscopic Approach
- Wisdom tooth extraction is performed under a therapeutic microscope providing precision and enhanced visibility.
- Wisdom tooth extraction combined with erbium chromium laser at 2780 nanometers, which prevents bone overheating and accelerates the healing process.
- Minimally invasive surgical technique resulting in rapid patient recovery and healing.
- Extraction using specialized PIEZO-SURGERY equipment for bone cutting and release around the tooth with ultrasonic tips specifically designed for the discussed procedure. Complete control during extraction time and minimizing damage to soft tissues, including nerve damage.
- Use of the patient's own blood to create fibrin-rich platelets to encourage new blood vessel formation, resulting in rapid healing of the area after extraction.
- Use of absorbable sutures and/or micro-sutures to prevent tearing and/or injury to soft tissue.
- Minimal flap elevation and preservation of anatomical structures.
- CT imaging and advance planning and patient preparation before extraction.
- Option to perform extraction under general anesthesia or deep sedation.
- For patients with dental anxiety, options for reflexology or advance psychological preparation before or during extraction to reduce anxiety or psychological stress.
How is an Impacted Wisdom Tooth Extracted?
Impacted wisdom tooth extraction can be a complex and delicate procedure, preferably performed by an oral surgeon or qualified dentist. The process involves several stages:
- Anesthesia: The first step in wisdom tooth extraction is administering anesthesia, usually local anesthesia within the mouth. Sometimes intravenous sedation may be required, and in complex cases, general anesthesia might be necessary.
- Incision: The doctor makes an incision in the gum tissue to expose the tooth and surrounding bone.
- Bone Removal: If the tooth is partially or completely impacted, the oral surgeon may need to remove some of the bone surrounding the tooth to gain access and safely remove the tooth.
- Sectioning: If the tooth is too large or deeply rooted to be removed whole, the doctor may need to section the tooth into smaller pieces to facilitate removal.
- Extraction: Once the tooth is properly exposed, the doctor carefully extracts the tooth from its socket.
- Cleaning and Suturing: After tooth removal, the socket is cleaned to remove any debris or remaining tooth fragments. The doctor then sutures the incision.
- Recovery: After the procedure, the patient receives instructions, and the doctor may prescribe antibiotics and pain medications as needed.

Does Wisdom Tooth Extraction Hurt?
Wisdom tooth extraction is typically performed under local anesthesia, intravenous sedation, or general anesthesia, which means the area around the tooth is numbed and you should not feel pain during the procedure. However, you may experience pressure or discomfort during the tooth removal.
After the extraction, when the anesthesia wears off and the area begins to heal, you may experience some discomfort or pain. Your dentist will prescribe appropriate pain medications.
Some individuals may experience more pain or discomfort than others. This depends on factors such as the tooth's location, the complexity of the extraction, and individual pain tolerance. However, most people find that the discomfort is manageable with appropriate pain medication and proper home care.
Risks and Complications You Should Know About
As with any medical procedure, there are potential risks and complications associated with impacted wisdom tooth extraction.
- Pain and Swelling: Common after wisdom tooth extraction, typically subsiding within several days to a week.
- Bleeding: Common after wisdom tooth extraction, usually stopping within a few hours.
- Infection: A potential complication of wisdom tooth extraction. Your dentist may prescribe antibiotics to help prevent infection, and it's important to follow all post-surgical instructions to minimize infection risk.
- Nerve Damage: In rare cases, nerves in the jaw or mouth may be damaged during wisdom tooth extraction, leading to numbness or tingling in the lips, tongue, or cheeks. This is usually temporary but can be permanent in rare instances.
- Sinus Problems: If an impacted wisdom tooth in the upper jaw is located near the sinuses, extraction may lead to sinus issues such as sinus pain, pressure, or infection.
- Dry Socket: A condition where a blood clot doesn't form in the socket after extraction, or it becomes dislodged or dissolves, leaving the bone exposed. This delays healing and exposes the area to food debris, bacteria, and infection, potentially causing severe pain.
- Jaw Stiffness: Jaw stiffness or limited jaw movement may occur after wisdom tooth extraction but typically resolves within several days to a week.

Post-Extraction Care Instructions for Impacted Wisdom Teeth
Following impacted wisdom tooth extraction, it's important to follow your dentist's instructions to ensure proper healing and prevent complications:
- Bite down on the gauze placed over the extraction site for approximately 30 minutes after the procedure. If bleeding continues, replace with fresh gauze for another 30 minutes.
- Avoid rinsing or spitting for the first 24 hours as this may dislodge the blood clot and delay healing.
- Apply an ice pack to the outside of your cheek intermittently for the first 24 hours to reduce swelling.
- Take pain medications as prescribed by your dentist. Over-the-counter pain relievers such as ibuprofen or acetaminophen can be taken to manage pain.
- Eat soft, cold foods such as smoothies, yogurt, and ice cream for the first few days after the procedure. Avoid hard, chewy, or spicy foods that may irritate the extraction site.
- Avoid smoking and alcohol consumption for at least 24 hours after the procedure, as these can delay healing and increase infection risk.
- Rinse your mouth with salt water regularly and avoid brushing teeth for 24 hours after extraction.
- Follow any additional instructions given by your dentist, including taking antibiotics if prescribed.
Important to Remember!
There is a risk of side effects such as: bleeding, limited mouth opening, swelling, pain, and nausea. Our patients report that after one day they returned to full routine without swelling and/or pain.
The logic is simple: when extraction is performed using minimally invasive surgical technique, in an intelligent and non-traumatic manner with appropriate magnification and understanding of body biology, there's no reason the treatment should be painful and traumatic for the patient.