Dr. Ariel Savion has been an active dentist since 2007 and holds a dual Master’s degree from Germany in Laser Sciences and Dental Implantology. He has clinical expertise in laser periodontal therapy, microscopic surgery, and dental implant procedures.
He serves as the Medical Director of the dental corporation Savion Medical Center Ltd. and is the founder and owner of the prestigious master_implant educational club, dedicated to training dentists in advanced fields of dentistry.
In addition, Dr. Savion is the only certified instructor in Israel on behalf of the World Clinical Laser Institute in the field of laser dentistry.
Dr. Savion is an international researcher and lecturer and serves as a Key Opinion Leader (KOL) for leading medical companies in Israel and worldwide, specializing in laser dentistry, periodontology, and dental implantology.

What Is a Gum Recession?
Gum recession is a common condition typically triggered by localized or systemic inflammation. When the gum tissue pulls away from the teeth, the root surface becomes exposed—often revealing a visible boundary between the enamel and cementum. This exposure may lead to tooth sensitivity and a noticeable lengthening of the tooth crown due to the visible root surface.
To prevent gum recession, patients should maintain proper oral hygiene, including effective brushing twice a day and using interdental brushes to remove plaque between the teeth. Regular dental cleanings every three months are also recommended to support gum health.

Early Signs of Gum Recession You Shouldn’t Ignore
Gum recession occurs when gum tissue gradually detaches from the tooth surface, exposing the root. This condition often progresses over time if left untreated. Early detection can prevent discomfort and long-term complications. Warning signs:
- Heightened Sensitivity to Hot or Cold
This is often one of the first indicators. A sharp or burning sensation when consuming hot or cold foods and drinks may suggest gum recession, though it can also point to other dental issues such as a cracked tooth.
- Teeth Appearing Longer Than Usual
If certain teeth look longer than before, this could be due to gum tissue pulling away and exposing more of the tooth root.
- Bleeding While Brushing
Healthy gums should not bleed during brushing or flossing. Bleeding is often an early sign of gum inflammation, which may progress to recession if not addressed.
- Notches or Indentations at the Gumline
If you feel or see grooves where the tooth meets the gum, this may indicate gum recession.
- Changes in Gum Color
Healthy gums typically have a pale pink color. Redness, swelling, or discoloration may signal inflammation, potentially leading to recession.
What Causes Gum Recession?
There are multiple contributing factors to gum recession. These include age, genetics, periodontal disease, aggressive or obsessive brushing, tobacco use, hormonal fluctuations, orthodontic treatments, pregnancy, acute infections, poor oral hygiene, bruxism (teeth grinding), misaligned teeth, and improper bite forces. Oral piercings can also damage soft tissue and promote inflammation or bone loss, increasing the risk of recession.
Without timely diagnosis and treatment, gum recession can lead to periodontal pockets where bacteria accumulate, causing further tissue damage. Eventually, untreated gum recession may lead to tooth mobility and tooth loss, requiring more complex and costly restorative procedures.

How to Protect Your Smile: Preventing Gum Recession Through Daily Habits
Effective prevention begins with consistent and proper oral hygiene. The foundation of gum health lies in daily practices that minimize bacterial buildup and protect the gumline.
- Brush Correctly, Not Aggressively Brushing twice a day with a soft-bristled toothbrush using gentle, angled strokes toward the gumline helps remove plaque without damaging the tissue. Overbrushing or using excessive force can contribute to gum loss.
- Clean Between Teeth Daily Flossing or using interdental brushes is essential for reaching areas your toothbrush cannot. Bacterial plaque tends to accumulate between teeth, and its persistence often leads to gum inflammation and eventual recession.
- Routine Dental Visits Are Essential Regular check-ups and professional cleanings every three months help prevent tartar buildup, detect early signs of gum disease, and halt ongoing recession. These visits are especially important for patients with a history of periodontal issues.

Gingivitis vs. Gum Recession, all the Differences
Gingivitis is the early stage of gum disease characterized by redness, swelling, and bleeding. It’s primarily caused by plaque accumulation along the gumline. The good news is that gingivitis is reversible with improved oral hygiene and regular professional cleanings.
Gum recession, on the other hand, involves the physical loss of gum tissue, which exposes the tooth root. It represents a more advanced and often irreversible stage of periodontal damage. If not treated, it may lead to bone loss, tooth instability, and eventual tooth loss.
"Gingivitis and gum recession are separate but related conditions. Gingivitis is often the first warning sign and should not be ignored. Early intervention can prevent the progression to more serious gum damage."
Dr. Savion emphasizes

Traditional Surgical Approach: Free Gingival Graft (FGG)
The gold standard for treating gum recession has long been the Free Gingival Graft (FGG) procedure. This method involves harvesting a small section of soft tissue usually from the patient’s palate—and transplanting it to the site of recession.
Many patients are hesitant due to concerns about post-operative discomfort and the need for tissue harvesting. This has driven interest in alternative methods that avoid palatal grafting while still achieving predictable outcomes.
FGG remains highly effective, particularly in cases with minimal attached gingiva or significant tissue loss. However, advancements in microsurgery and laser-assisted techniques are offering patients less invasive options with quicker recovery and comparable clinical success.
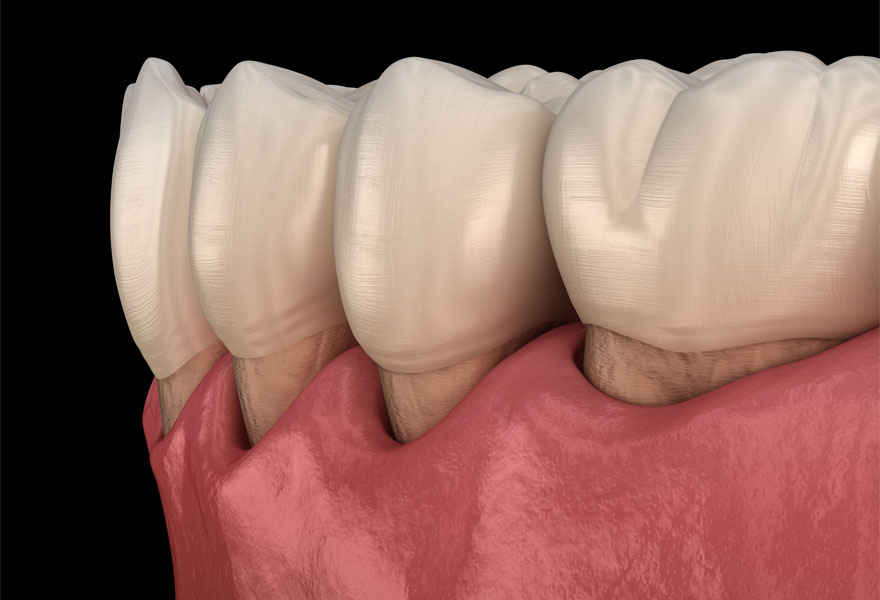
Recognizing Gum Recession: Diagnosis and Key Clinical Indicators
Diagnosing gum recession is typically straightforward, as the condition presents with clear and recognizable signs:
- Bleeding during brushing or spontaneously throughout the day
- Sensitivity to temperature changes, especially hot or cold foods
- Swollen or reddened gums
- Roots visibly exposed or teeth appearing longer than usual
- Persistent bad breath
While any general dentist can identify gum recession, referral to a periodontist is often advisable for a more precise assessment. A specialist can determine the underlying cause whether it’s infection, chronic inflammation, poor hygiene, caries, smoking, or other systemic factors and formulate a targeted treatment plan.
Look at this amazing transformation: From Gum Problems to a Perfect Smile
Nutrition and Gum Health: Why Diet Matters in Periodontal Care
A well-balanced diet helps the body resist infection and supports the healing of soft and hard tissues.
Deficiency in essential nutrients may compromise the oral microbiome and reduce the body’s ability to respond to bacterial threats. Diets high in sugar and refined carbohydrates contribute to acid production, enamel erosion, and increase the risk of cavities and periodontal disease.
In addition, poor dietary habits can fuel the growth of pathogenic bacteria that damage periodontal structures. This leads to inflammation, formation of periodontal pockets, and eventual tooth loss if untreated.
Patients with gum disease or those recovering from gum procedures should focus on a nutrient-rich diet to support healing and long-term stability.
Pinhole Technique (PST): Widely Publicized, But Not for Every Case
The Pinhole Surgical Technique (PST), developed by California-based periodontist Dr. John Chao, is a minimally invasive method for treating gum recession. It requires no tissue harvesting from the palate, no releasing incisions, and no sutures. The method has gained significant exposure in U.S. media and online platforms, largely due to Dr. Chao’s active promotion and the endorsement of clinicians trained in his technique. As a result, many patients inquire specifically about PST without being aware of other clinically proven options and without understanding its limitations.
PST is designed to cover exposed roots, but The thickness of the soft tissue must be evaluated beforehand. For patients with thin gingival biotypes, this method is generally not recommended, as long-term success depends on adequate tissue bulk to maintain coverage. Additionally, clinicians must assess the relationship between the bone crest and the gum margin using the Miller classification to estimate the likelihood of success.
The procedure involves a single small incision above the root. Through this access point, specialized instruments are used to gently release the tissue from the bone and reposition it coronally. In cases requiring additional volume, allogeneic or xenogeneic graft material may be inserted still without the need for sutures.
While PST offers advantages in terms of reduced invasiveness, it is not suitable for every patient. Those with generalized recession, thin, soft tissue, strong muscle pull, or a shallow vestibule may not benefit from this approach. For this reason, periodontists must be well-versed in all available techniques and select the most appropriate method based on each patient’s anatomical and clinical profile. The key limitation of PST lies in its narrow indication range.
The Tunneling Method for Root Coverage
One of the most established microsurgical approaches to covering gum recession is the tunneling technique. Developed by German clinicians Dr. Markus Hürzeler and Dr. Otto Zuhr, this method minimizes trauma by avoiding vertical incisions and flap elevation.
Instead, the gum tissue is gently separated from the underlying bone through a small tunnel-like access, allowing it to be advanced coronally (toward the crown). In selected cases, a connective tissue graft is inserted into the tunnel to thicken the gum and provide long-term coverage. Sutures are anchored at contact points to hold the tissue in position.
This technique is known for its aesthetic outcomes and reduced post-operative discomfort. However, it may not be suitable for patients with thin gingival biotypes, as the tissue is more prone to tearing during mobilization.
VISTA Technique: Vertical Access for Precise Root Coverage
The Vestibular Incision Subperiosteal Tunnel Access (VISTA) technique is another microsurgical approach for treating gum recession. Developed by California-based periodontist Dr. Homa Zadeh, the method involves creating a single horizontal incision in the vestibule, typically in the frenum area, followed by a subperiosteal dissection that allows for coronal repositioning of the soft tissue.
Once the tissue has been sufficiently mobilized, it is passively advanced over the exposed roots and stabilized with sutures placed in the central portion of the affected teeth. In cases of thin soft tissue, a connective tissue graft may be harvested and secured using sutures, or platelet-rich fibrin (PRF) may be inserted to enhance volume and healing.
The VISTA technique has demonstrated strong clinical outcomes and aesthetic success. However, similar to other tunneling-based methods, it may not be ideal for patients with very thin gingival biotypes, as the tissue is more prone to tearing during mobilization.
Coronally Advanced Flap (CAF): A Versatile and High-Precision Method
The Coronally Advanced Flap (CAF) technique, introduced by Italian periodontist Prof. Giovanni Zucchelli, is considered one of the most precise and effective surgical approaches for root coverage.
The procedure begins with a partial-thickness flap elevation without disrupting the interdental papillae. The soft tissue is carefully released from underlying muscle attachments to allow for passive coronal advancement. In cases with insufficient tissue thickness, a thin connective tissue graft harvested from the palate at a depth of approximately 0.7 mm is placed at the recession site.
The graft is then stabilized using a specialized suturing technique that results in a dual-layered soft tissue structure, effectively reinforcing the gingival margin.
CAF can be applied across a wide range of clinical cases, including severe recession. It offers excellent long-term outcomes in both function and aesthetics. One of the key advantages of this method is that over time, the quality and thickness of the gingival tissue improve, reducing the likelihood of recurrence. This technique is widely regarded as a benchmark in periodontal plastic surgery.
Laser-Assisted Microsurgery for Gum Regeneration and Root Coverage
In complex cases of gum recession, advanced microsurgical treatment using laser technology can offer significant benefits. This technique combines precision soft-tissue manipulation with biologic stimulation under high magnification using a dental microscope.
Dr. Savion applies a multi-phase approach:
- Laser-Assisted Pocket Reduction Targeted laser energy is used to remove diseased tissue, sterilize periodontal pockets, and eliminate bacterial biofilm. This minimally invasive procedure avoids cutting and reduces post-operative discomfort.
- Tissue and Bone Regeneration In areas where bone and soft tissue have been lost, regenerative materials are applied after laser decontamination. These materials promote the body’s natural healing response and support the reconstruction of periodontal structures.
- Gum Grafting With Emdogain In severe cases, soft-tissue grafts are placed, typically using a superficial palatal harvest. Emdogain, a biologically active protein-based gel, is applied to the root surface prior to grafting to enhance integration and tissue attachment.
What Is Emdogain and How Does It Work?
Emdogain is a biologically active gel derived from enamel matrix proteins, primarily amelogenins. These proteins play a crucial role in tooth development and attachment during early childhood. When applied to a cleaned root surface during periodontal surgery, Emdogain stimulates the regeneration of key supporting tissues, including cementum, periodontal ligament, and alveolar bone.
Clinical studies have confirmed its safety and effectiveness. Approved by the FDA, the European Union, and Israel’s Ministry of Health, Emdogain is widely used in periodontal therapy to promote soft tissue adhesion, bone formation, and long-term tooth stability.
In gum grafting procedures, Emdogain enhances graft integration and helps re-establish the biological connection between the tooth root and the surrounding tissues. It not only accelerates soft tissue healing but also significantly improves the predictability of clinical outcomes in challenging cases of gum recession.

תמונה עליונה - מצב התחלתי עם נסיגת חניכיים באזור קדמי תחתון, באזור הניבים ובאזור המלתעות. במקרה הנ״ל, צחצוח אגרסיבי גרם לנסיגת חניכיים. עקב משיכת שרירים חזקה בזמן הדיבור, נבחרה שיטת CAF לכיסוי הרצסיות.
תמונה תחתונה - מעקב לאחר 6 חודשים, ניתן להתרשם מכיסוי מלא של השורשים, עם עובי רקמה בריאה עם תוצאה אסתטית ללא סימן לשתלי חניכיים. במקרה הזה, נעשה שימוש בחלבון אמדוגן לרגנרציה פריודונטלית. הלסת חולקה לשלושה חלקים ובכל טיפול בוצע חלק אחד. כפי שציינתי לעיל, שיטה זא דורשת טיפול תחת מיקרוסקופ טיפולי ומיומנות רופא פנומנאלית כדי להגיע לתוצאות טובות, לכן רבים מהרופאים זונחים את השיטה ובוחרים בשיטות קלות יותר (כמו טכניקת pinhole שלא מצריכה חתכי שחרור, לא מצריכה קצירה והשתלת חניכיים ותפרים, יחד עם זאת, לא תתקבל אותו תוצאה) אך לא בהכרח נכונות למקרה הספציפי.
Facts About Tooth Brushing: What Patients Should Really Know
Effective brushing is a cornerstone of oral health, yet many people overlook the importance of proper technique and consistency. The following facts highlight why brushing is more than just a routine habit:
- The average person spends approximately 38 days of their life brushing their teeth.
- Modern toothpaste formulations only became common about a century ago. Prior to that, substances like tobacco, honey, and lemon juice were used.
- Nearly 25% of Israelis report brushing only once a day—significantly below recommended standards.
- Brushing after breakfast, rather than immediately upon waking, is more effective in removing food particles and acids that accumulate during meals.
- Circular brushing motions angled toward the gumline with moderate pressure are more effective than harsh horizontal strokes.
- The optimal brushing time is two minutes per session. Supplementing with interdental brushes and non-medicinal mouthwash improves overall cleanliness.
- Plaque starts forming within 24 hours of missed brushing, increasing the risk of decay and gum disease.
- Brushing immediately after vomiting can lead to enamel erosion due to the acidic environment. It's best to rinse with water and wait before brushing.
- Nighttime brushing is especially critical. Saliva production drops during sleep, reducing its natural protective effect and allowing bacteria to proliferate.
- Poor oral hygiene is linked to increased cardiovascular risk. Studies show that individuals who brush less frequently are up to 70% more likely to develop heart disease due to systemic inflammatory responses.

Post-Treatment Guidelines: Supporting Healing and Long-Term Results
Dr. Savion recommends the following:
- Brush twice daily using a soft-bristled toothbrush with gentle technique.
- Maintain excellent oral hygiene, including interdental cleaning.
- Visit the dental hygienist for professional cleaning every three months.
- Schedule annual evaluations with the treating dentist to monitor healing and detect potential relapse early.
A Tailored, Evidence Based Approach to Gum Recession Treatment
Successful treatment of gum recession requires accurate diagnosis and individualized care. There is no single method suitable for every patient. Dentists and periodontists must be trained in a range of techniques and apply the one most appropriate for the patient’s specific condition.
Patients experiencing signs of gum recession should consult a clinic that specializes in laser-assisted periodontal therapy. Early intervention combined with modern surgical tools increases the likelihood of preserving natural teeth and avoiding more complex procedures.
Dr. Savion's approach integrates advanced diagnostics, laser technology (he holds a master’s degree in Laser Science), microsurgical techniques, and regenerative materials such as Emdogain. When applied correctly and based on clinical evidence, these tools significantly enhance outcomes even in severe cases.
"Strategic planning is the foundation of successful periodontal care."
As Dr. Savion states: