What Causes Gum Disease?
The primary cause of gum disease is bacterial infection originating in dental plaque – the sticky biofilm that accumulates on teeth and gums.
Several factors contribute to the development of periodontal disease:
- Poor oral hygiene – Inadequate brushing or flossing allows plaque to accumulate. Over time, plaque hardens into tartar, which cannot be removed by brushing and provides a favorable environment for bacterial growth.
- Bacterial infection – The bacteria in plaque release toxins that irritate the gums, leading to gingivitis – the initial stage of gum disease. Without treatment, this can progress to periodontitis, affecting the bone and connective tissue supporting the teeth.
- Smoking and tobacco use – Tobacco weakens the immune response and reduces blood flow to the gums, slowing healing and increasing susceptibility to infection.
- Genetic predisposition – Some individuals are more genetically prone to gum disease, making their gum tissues more sensitive to bacterial effects.
- Hormonal changes – Hormonal fluctuations during puberty, pregnancy, or menopause can make gums more reactive and prone to inflammation.
- Systemic conditions and medications – Diseases such as diabetes or autoimmune disorders can influence gum health. Medications that reduce saliva flow also contribute to gum problems by decreasing the mouth’s natural protective effects.
- Poor nutrition – A diet lacking essential vitamins and minerals weakens the immune system and impairs tissue repair.
Dr. Ariel Savion has been an active dentist since 2007 and holds a dual Master’s degree from Germany in Laser Sciences and Dental Implantology. He has clinical expertise in laser periodontal therapy, microscopic surgery, and dental implant procedures.
He serves as the Medical Director of the dental corporation Savion Medical Center Ltd. and is the founder and owner of the prestigious master_implant educational club, dedicated to training dentists in advanced fields of dentistry.
In addition, Dr. Savion is the only certified instructor in Israel on behalf of the World Clinical Laser Institute in the field of laser dentistry.
Dr. Savion is an international researcher and lecturer and serves as a Key Opinion Leader (KOL) for leading medical companies in Israel and worldwide, specializing in laser dentistry, periodontology, and dental implantology.

Stages and Types of Gum Disease
Stages of Gum diseases:
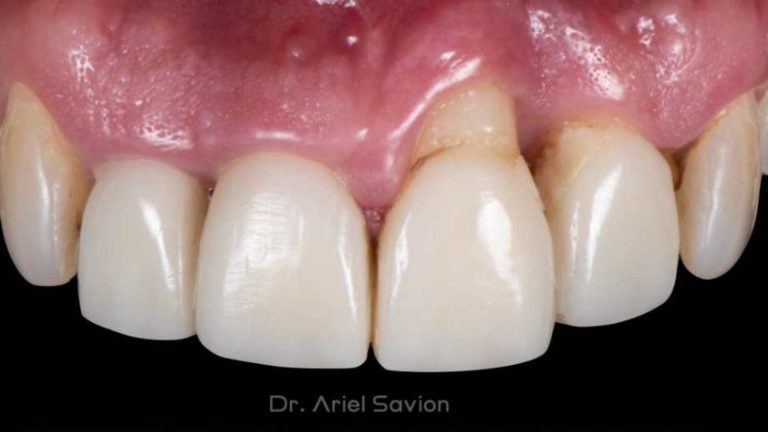
- Gingivitis – The earliest and mildest form, characterized by redness, swelling, and bleeding during brushing or flossing. At this stage, damage is limited to the gums and can be reversed with proper care.
- Periodontitis – When gingivitis is untreated, it advances to periodontitis, where the supporting bone and connective tissues are damaged.
- Mild periodontitis – Slight bone loss and early gum recession. Small pockets may form between the teeth and gums.
- Moderate periodontitis – Deeper pockets and more noticeable gum recession. Teeth may become sensitive or slightly mobile.
- Severe periodontitis – Significant bone loss, advanced gum recession, and loose or shifting teeth. The damage to supporting structures may become irreversible.

Post-Surgical Care and How to Maintain Healthy Gums
After gum surgery:
- Follow post-operative instructions – Adhere to your dentist’s guidelines.
- Maintain good oral hygiene – Use a soft-bristled toothbrush and brush gently. Rinse with antimicrobial mouthwash or saltwater as directed. Avoid vigorous rinsing, spitting, or flossing near the treated area during the initial healing phase.
- Balanced nutrition – Eat foods rich in vitamins and minerals, especially vitamin C, to support healing and tissue repair. Avoid hard, crunchy, or spicy foods that may irritate the surgical site.
- Manage discomfort and swelling – Some soreness or swelling is expected. Follow your dentist’s pain management instructions. Applying ice to the outside of the face can reduce swelling. Avoid very hot or cold foods and drinks to minimize sensitivity.
- Avoid smoking and tobacco – Smoking restricts blood flow and slows healing, increasing the risk of complications.
The Precision of Dental Lasers and Targeting Bacteria with Accuracy
The precision of dental lasers is one of their main advantages compared to conventional gum surgery.
Selective and Controlled Treatment, Laser-assisted periodontal procedures precisely target diseased tissue without affecting the surrounding healthy areas. This selective action allows for accurate removal of infected gum tissue and bacteria, minimizing unnecessary trauma to adjacent tissues.
Bacterial Reduction, Laser energy effectively destroys bacteria within periodontal pockets. The light energy disrupts bacterial cell walls, leading to bacterial destruction and disinfection of the treated area. This reduces infection risk and promotes gum healing.
How Lasers Treat Gum Disease?
Dental lasers work by directing a concentrated beam of light at the affected gum tissue. The specific wavelength determines how the energy interacts with the tissue.
Absorption of Laser Energy, Gum tissues absorb the laser light mainly through pigments such as melanin and hemoglobin.
Photothermal Effect, Once absorbed, the laser energy converts to heat, which produces several biological effects:
- Bacterial destruction – The generated heat destroys bacteria in the periodontal pockets and infected areas by damaging their cell walls.
- Tissue removal (ablation) – The laser’s heat causes water in the diseased tissue to evaporate, allowing precise removal of infected or inflamed tissue.
- Coagulation and hemostasis – The laser seals small blood vessels during the procedure, reducing bleeding and providing a clear view for the dentist.
- Stimulation of healing and regeneration – Laser energy can activate cells in the gum tissue to produce collagen and growth factors, promoting regeneration and reattachment of gums to the tooth surface.
Technological Innovations in Periodontal Treatment
Several technological advancements are transforming gum disease management in modern dentistry.
Laser Dentistry – Laser systems enable minimally invasive treatment for various dental conditions, including caries removal, gum contouring, and periodontal therapy. They provide efficient results with less discomfort and faster recovery.
Digital X-Rays – Digital radiography offers detailed visualization of teeth and supporting bone, allowing more accurate diagnosis and treatment planning. Images can be easily shared with specialists.
Cone Beam CT Scans – These scans provide 3D views of teeth, bone, and soft tissues, assisting in precise implant placement, bone evaluation, and diagnosis of periodontal disease.
Intraoral Cameras – Handheld cameras capture detailed images of teeth and gums, improving visibility of hard-to-reach areas and enabling early detection of issues.
3D Printing Technology – Used to produce customized implants, bridges, and dentures, 3D printing enhances fit and function while reducing waiting time and improving surgical planning.
Artificial Intelligence (AI) – AI algorithms analyze patient data to improve diagnosis and treatment planning, identify early signs of oral disease, and simulate virtual treatment outcomes for better clinical decision-making.
Common Types of Lasers Used in Dentistry
Dental lasers are classified according to the type of tissue they target – soft tissue or hard tissue.
Soft Tissue Lasers:
- Diode Laser – Commonly used for crown lengthening and treating gum disease. It allows precise and safe removal of inflamed gum tissue.
- Erbium Laser – Suitable for both soft and hard tissues. Used for periodontal therapy, caries removal, and tooth surface preparation before restorations.
- CO₂ Laser – Used for soft-tissue procedures such as removing oral lesions, treating ulcers, and performing minor oral surgeries. It is highly effective for cutting and vaporizing soft tissue.
Hard Tissue Lasers (Erbium-based types):
- Er:YAG Laser – Primarily used for hard-tissue applications, including cavity preparation, decay removal, and bone reshaping during surgery.
- Nd:YAG Laser – Applied in both periodontal and endodontic treatments, including root canal disinfection and soft-tissue decontamination. It has strong antibacterial properties and is suitable for both soft and hard tissues.

When Laser Treatment May Not Be Suitable?
Laser dentistry is not ideal for all clinical cases.
- Tooth structure and restorations - Some teeth with ceramic or reflective restorations may not respond effectively to laser energy.
- Severe periodontal disease - In advanced cases, laser therapy alone may be insufficient. Conventional treatments such as scaling, root planing, or surgical intervention may be necessary.
- Medical conditions and pregnancy - Dentists must review a patient’s overall health and medical history to determine whether laser use is appropriate and safe.
The REPAIR Protocol with Er,Cr:YSGG Laser
Thar are two main patient groups:
- Patients with dental implants who develop peri-implant soft-tissue infections -either peri-mucositis (limited to soft tissue) or peri-implantitis (involving bone loss).
- Patients with natural teeth suffering from periodontal disease of varying severity, regardless of age or gender.
Dr. Savion: "many such cases recur because the initial treatment was incomplete, improper tools were used, or post-treatment maintenance was insufficient. As a result, patients often relapse to the original stage of disease."
Gum disease significantly affects quality of life – it can cause bad breath (halitosis), gum recession, tooth mobility due to bone loss, discomfort, and in severe cases, loss of the natural bite due to the destruction of periodontal support.
The BIOLASE REPAIR Protocol:
Developed by BIOLASE, a leading American company in dental laser research, the REPAIR protocol is designed for periodontal disease treatment of varying severity.
It is a minimally invasive surgical approach that combines laser therapy with dental microscopy. The method focuses on preserving natural teeth for the long term and promoting periodontal regeneration – the renewal of gum and supporting tissues.
The REPAIR Protocol for Scaling and Root Planing with Laser Energy
Laser-assisted periodontal therapy compared to traditional surgical procedures:
- It is a non-surgical procedure in most cases, eliminating the need for scalpels, sutures, or flap surgery.
- Local anesthesia is usually sufficient, and the treatment can often be completed in a single visit.
- The treatment is simpler and more comfortable for patients, minimizing bleeding and improving visibility in the treatment area.
- In most cases, patients prefer a closed, laser-assisted surgical approach (without flap elevation), which avoids stitches, postoperative discomfort, and gum recession.
- The laser’s 14 mm tip, combined with a dental microscope, can reach deep into periodontal pockets, remove infected tissue and calculus with precision, and promote faster healing.
- The procedure is minimally invasive, results in little or no bleeding, reduces pain, and enables quicker recovery.

The Er,Cr:YSGG Laser Protocol (2780 nm)
The Er,Cr:YSGG laser is designed for both hard and soft tissue applications. It can treat enamel, dentin, bone, titanium (on implants), and soft gum tissue.
The purpose of this protocol is to guide clinicians step-by-step in treating periodontal disease – whether in its early, moderate, or advanced stages – through a standardized, evidence-based process.
- Greater comfort and shorter chair time for patients.
- Minimally invasive, micro-surgical technique that reduces pain and postoperative discomfort.
- Minimal bleeding, or none at all, during the procedure.
- Conservative approach – the laser does not damage the tooth’s root cementum, unlike conventional scaling and root planing with manual or rotary instruments.
- No incisions or sutures are needed; gum flaps are not raised, which preserves natural anatomy.
- Faster healing and rapid return to normal activities without swelling or significant pain.
Clinical Stages of the REPAIR Protocol
The REPAIR protocol consists of three phases:
- Pre-surgical phas
- Surgical phase
- Post-surgical phase
Phase A – Pre-Surgical Assessment
All patients must undergo a full periodontal examination, including a periodontal charting, evaluation of pocket depths, and a comprehensive medical and family history review (including any genetic predisposition to gum disease).
Initial therapy includes scaling and root planing above and below the gumline, patient education on oral hygiene, and instruction in the use of interdental brushes. An evaluation of occlusion, tooth mobility, and the need for stabilization should also be performed.
Phase B – Surgical Procedure
After pre-surgical cleaning and scaling, the clinician re-evaluates the condition of the gums, ensuring the patient maintains proper oral hygiene using a soft-bristled electric toothbrush. Pocket depth measurements and gum response to initial treatment are reviewed.
The procedure then proceeds as a closed-flap laser surgery, performed with an Er,Cr:YSGG laser under a dental microscope for maximum precision.
The following steps summarize the surgical sequence:
- External pocket de-epithelialization – Using the laser to peel a thin epithelial layer from the outer gingival surface down to the pocket base.
- Gingivectomy (if needed) – Removal of excess soft tissue in cases of pseudo-pockets to restore proper contour while maintaining the biological width.
- Internal de-epithelialization and pocket debridement – Removal of the inner epithelial lining and release of the gum margin to gain better access to the pocket and subgingival calculus. The microscope enhances precision and visualization.
- Scaling and root planing – Thorough cleaning of the root surface using ultrasonic instruments under magnification, followed by chlorhexidine irrigation.
- Granulation tissue removal – Laser removal of inflamed and granulated tissue, exposing bone for regeneration and reattachment of healthy connective tissue.
- Bone decontamination and reshaping – Using a different laser tip, the bone defect is gently smoothed and reshaped parallel to the tooth root without causing damage.
- Final debridement and hemostasis – Stabilization of a clean blood clot within the treated area to promote rapid healing.
- Placement of fibrin membrane and compression – Application of a fibrin membrane to support tissue regeneration and protect the surgical site.
Phase C – Post-Surgical Care
Immediately after surgery, patients should brush only with an ultra-soft postoperative toothbrush designed for gum surgery. The dentist typically recommends chlorhexidine mouth rinses twice daily for 10 days to control bacteria and support healing.
After one week, gentle cleaning can begin using interdental brushes with soft bristles. The treated area should not be probed for pocket depth for at least three months following surgery to avoid tissue disruption. After three months, a follow-up cleaning and removal of supragingival calculus are performed to maintain long-term gum health.