Clinical case presented by Dr. Ariel Savion, D.M.D, LL.B, M.Sc, I.C.O.I
Introduction
Etiological treatment of peri-implantitis under a microscope aims to reduce the bacterial load within the peri-implant pocket and decontaminate it with erbium and chromium: An Er,Cr:YSGG laser (2780 nm) is used on the implant surface to promote osseointegration. Implant surfaces have changed from machined titanium to rough surfaces. Rough implant surfaces enhance implant stability in the bone, but they may create an environment for increased plaque and bacterial colonization, resulting in peri-implantitis.
Undoubtedly, microscope-enhanced periodontal and implant therapy, has reshaped clinical practice and created the potential for a higher standard of care. A microsurgical approach improves tissue preservation and handling while using specific flap design to access the defects in peri-implantitis treatment.
Definition peri-implant mucositis: Reversible inflammation of the soft tissues surrounding implants If such an inflammation is combined with loss of bone, it is referred to as peri-implantitis. Peri-implantitis, if not treated successfully, may lead to a complete loss of osseointegration and implant loss. The better we see, the more precise our data for the diagnostic result. The use of a microscope enables dentists to find a greater number of efects than with either magnifying loupes or the naked eye. Peri-implantitis may occur due to both biological and mechanical factors. It can be treated by a variety of methods. In the present case report, treatment was attempted by regenerative osseous surgery associated with an Er,Cr:YSGG laser (Biolase, USA) under magnification (ZEISS EXTARO 300, Carl Zeiss Meditec AG, Germany).
Medical and dental anamnesis
Patient motive: A 52-year-old, non-smoking male complained of suppuration and bleeding around an implant 2.2 in the area of the upper left lateral incisor.
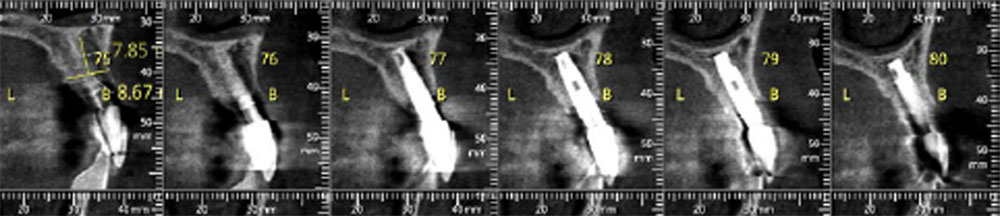
Clinical examination: After clinical examination and radiographs, it was found that there was a 2 mm recession, a probing depth of 8 mm, mobility grade one, and mesial and distant bone loss.
Medical history: Healthy and non-smoking patient had no specific local or systemic disease that could affect the treatment.
Diagnosis: Clinical examination of the implant site under magnification by eriodontal probe revealed a buccal probing depth of 8 mm, buccal recession of 2 mm, while bleeding on probing and exuding pus. The buccolingual crown mobility was less than 2 mm. The width of keratinized tissue was 3 mm and it had a thick biotype. By examining the occlusion, it was found that there was no heavy occlusion or overloading at the implant site. The patient had maxillary midline shift to the right. Therefore, a poor prosthesis design resulted in patient dissatisfaction and esthetic failure. Radiographs CBCT revealed bone loss to the level of 3 mm around the implant.

Aims: Peri-implantitis, if not treated successfully, may lead to a complete loss of osseointegration and implant loss. Failure of peri-implantitis treatment may happen as the result of patient-related factors, such as having systemic conditions that may delay wound healing and being a smoker, or procedure-related factors. With regard to procedure-related factors, treatment failure may result from incomplete decontamination or detoxification of the implant surface, an increase
in temperature of the implant site, a change in the implant surface roughness, or a failure to improve the titanium biocompatibility. In addition, unsuitable or insufficient bone graft materials may result in treatment failure. In the present case report an Er,Cr:YSGG laser was used to perform the flap incisions, decontaminate the defect site and the implant surface, and perforate the bone under magnification. A microsurgical approach with the ZEISS EXTARO 300 improves visualization during laser decontamination and optimizes flap mobility to achieve primary closure after bone and/or tissue augmentation. This microsurgical approach reduces trauma caused to the tissue by enabling the use of smaller suture diameters. Furthermore, it reduces the tension applied to the tissue margin during wound healing. These advantages are especially useful when dealing with fragile tissues with a limited vascular network such as the interdental mucosa. The use of ZEISS EXTARO 300 improves surgical access to interplant space. It is also important to mention that in the augmented visualization modes, Green Color Mode is used to enhance image contrast between blood and tissue so that they can be better distinguished.
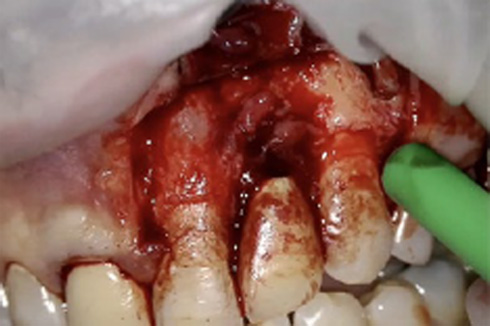
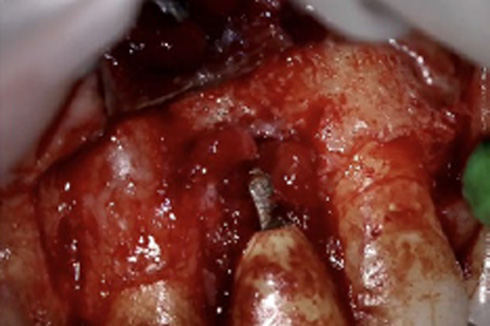
Fig. 2 – Peri-implantitis after mucoperiosteal flap with vertical releasing incision
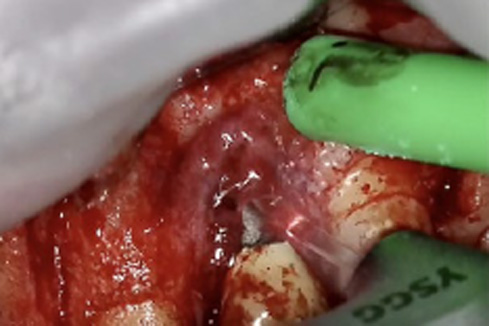

Fig. 3 – Granulation tissue removal with Er,Cr:YSGG laser – Tip MC3
Laser parameters: A full-thickness flap was performed using an Er,Cr:YSGG laser (2.5 W, 50% water, 50% air, and frequency of 50 Hz in a pulsed mode using a T4 tip of 400 µm in diameter). Granulation tissue was removed with settings of 2.5 W, 20% water, 20% air, and frequency of 30 Hz in a contact mode using an MZ-6 Tip with a 600 µm in diameter. Bone perforations at the buccal cortical plate adjacent to the defect were performed using an MZ- 6 Tip, 4.5 w, 90% water, 60% air, and frequency of 20 Hz in non-contact mode.


Fig. 4 – Abutment removal
Implant surface debridement was performed in non-contact mode, using an MZ-6 tip of 600 µm in diameter at 1.25 W, 80% water, 60% air, and frequency of 50 Hz in a direction perpendicular to the implant surface and 5 mm from the implant surface. The area was copiously irrigated with normal saline.


Fig. 5 – Granulation tissue removal with Tip MZ6, 14 mm length
Treatment: Local anesthesia was given (2 ml Articaine hydrochloride 4% with 1/100,000 adrenaline). The patient and operating staff wore special Er,Cr:YSGG laser–protective eyeglasses. Highly reflective instruments or instruments with mirrored surfaces were avoided during laser beam application (to avoid reflections of the laser beam). After flap reflection, it was found that the buccal cortical plate had resorted to about 3 mm, and fibrous granulation tissue was present on the three-dimensional sides of the implant. Granulation tissue was removed using the laser. After complete removal of the fibrous granulation tissues, the osseous defects became clear to the third implant ration. Therefore, the defect was a combined osseous defect.

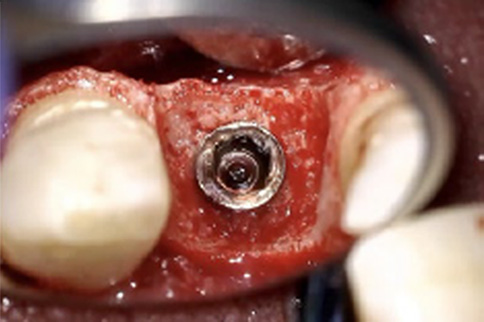
Fig. 6 – Three-dimensional view around implant
Regenerative osseous surgery was performed using an Er,Cr:YSGG laser (2,780 nm) at different settings to open the flap, remove the granulation tissue, perforate the bone, and clean the implant surface. A bone graft and a bioabsorbable membrane were used for bone regeneration.

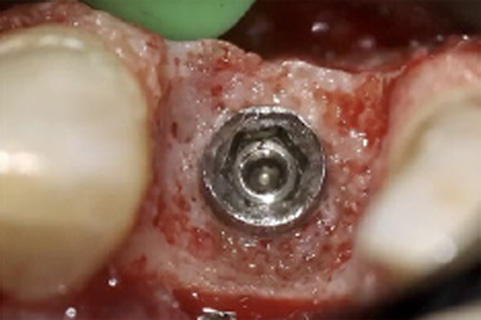
Fig. 7 – Laser emission inside of implant for decontamination
A bone graft (0.25 mm to 1 mm granules) and a bioabsorbable collagen membrane as GBR were used to fill the osseous defects and to cover the exposed implant surface. The crown was replaced with a new zirconia abutment and cemented crown made of monolithic zirconia, which met the patient’s expectations in terms of shape, dimensions, and color.
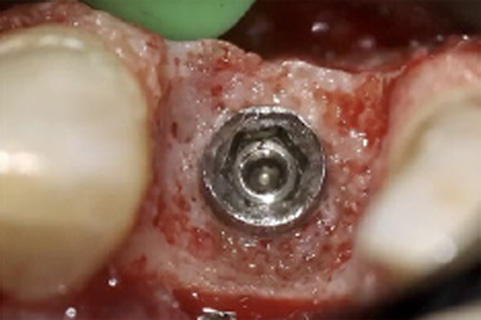

Fig. 8 – Guided bone regeneration
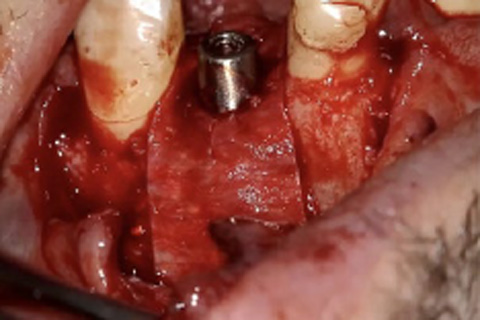

Fig. 9 – Suture 5/0 nylon
Post-operative recommendation: Amoxicillin, 500-mg capsules, three times daily for seven days and Ibuprofen, 400-mg tablets, as needed were prescribed for the patient. The patient was instructed to avoid eating hot food for the first 24 hours. Normal oral hygiene procedures were performed by the patient using a soft brush and 0.12% chlorhexidine mouthwash. Sutures were removed after 10 days.


Fig. 10 – After 10 days
Conclusion: At three, six, and 12 months postoperatively, there was no reported complication, with probing depths of 3 to 5 mm, less than 1 mm recession, no bleeding loss or implant mobility, and good bone formation. The optimal result of peri-implantitis treatment is regeneration of the lost implant supporting hard and soft tissue.


Fig. 11 – Healing after 3 months


Fig. 12 – Before final restoration
Microsurgical concept
To ensure proper treatment, which is a fundamental requirement in implant therapies, the required information must be obtained by clinical examination under magnification with additional appropriate image-guided diagnostics. Development of microscopes like the ZEISS EXTARO 300, refinement of surgical instruments, development of improved sutures materials, and training in the microsurgical field (Microscopic Dental Club) all play a role in the worldwide establishment of microsurgical technique. Magnification, illumination, and instrumentation are the three elements referred to as
the microsurgical triad. For improving accuracy in surgical intervention, the former elements are prerequisites in the microsurgical field. Without any of these, microsurgery is not possible.


Fig. 13 – Zirconia abutment


Fig. 14 – Final restoration
Augmented visualization modes in ZEISS EXTARO 300 in microsurgical concept: In order to avoid unfavorable metallic glare under illumination from ZEISS EXTARO 300, we can use augmented visualization in the form of the NoGlare mode. Furthermore, the instruments should have a colored coating surface. Suture materials and techniques are essential factors to consider in microsurgery. Wound closure is a key prerequisite for healing following surgical interventions and most important to avoid complications. A wound may significantly enhance the susceptibility to infection.
Needle and thread characteristics also influence wound healing and surgical outcomes. The magnification recommended for surgical intervention ranges from 2.5x to 39x.
In implantology, magnification of 4x to 6x for loupes and 1.4x to 29x for ZEISS EXTARO 300 appear to be ideal depending on the kind of intervention. Nevertheless, the depth of field decreases with increased magnification.

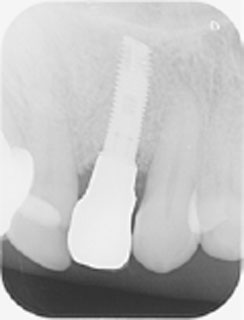
Fig. 15 – Final outcome
To achieve proper regeneration, a few factors should be considered. These factors include sterilization of the wound site, defect size and topography, space maintenance, graft immobilization, primary soft tissue closure, rapid revascularization, and sufficient healing time. Therefore, complete regeneration of peri-implant defects can only be ensured with the use of bone graft materials following implant surface decontamination.


Fig. 16 – Left: Before bone regeneration (10x); right: 10-day healing period (suture 6/0 monofilament, non reservable)
An Er,Cr:YSGG laser under the ZEISS EXTARO 300 was highly efficient and effective in removing contaminants from the implant body without overheating or altering the surface characteristics of the roughened titanium surface. The absence of any measurable changes to the titanium surface and the lack of an organic smear layer creates the ideal environment for the regrowth of bone and potential reintegration of the exposed or contaminated area of the implant body. The Er,Cr:YSGG laser enabled regenerative osseous surgery around the implant with no complications as well as with high patient and clinician satisfaction and confidence during the 12-month follow-up period.


Fig. 17 – Left: Soft tissue before final restoration; right: Final zirconia monolithic crown